(Total Views: 672)
Posted On: 01/24/2022 6:24:53 PM
Post# of 157004

Coronavirus (COVID-19) Update: FDA Limits Use of Certain Monoclonal Antibodies to Treat COVID-19 Due to the Omicron Variant
The following is attributed to Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research
As we have throughout the COVID-19 pandemic, the U.S. Food and Drug Administration has used the best available science as the virus has evolved to make informed decisions with the health and safety of the American public in mind. Ensuring that healthcare providers on the frontlines have the best tools available to treat patients is a top priority for the agency.
In light of the most recent information and data available, today, the FDA revised the authorizations for two monoclonal antibody treatments – bamlanivimab and etesevimab (administered together) and REGEN-COV (casirivimab and imdevimab) – to limit their use to only when the patient is likely to have been infected with or exposed to a variant that is susceptible to these treatments.
Because data show these treatments are highly unlikely to be active against the omicron variant, which is circulating at a very high frequency throughout the United States, these treatments are not authorized for use in any U.S. states, territories, and jurisdictions at this time. In the future, if patients in certain geographic regions are likely to be infected or exposed to a variant that is susceptible to these treatments, then use of these treatments may be authorized in these regions.
Monoclonal antibodies are laboratory-made proteins that mimic the immune system’s ability to fight off harmful pathogens such as viruses, like SARS-CoV-2. And like other infectious organisms, SARS-CoV-2 can mutate over time, resulting in certain treatments not working against certain variants such as omicron. This is the case with these two treatments for which we’re making changes today.
Based on Centers for Disease Control and Prevention data, the omicron variant of SARS-CoV-2 is estimated to account for more than 99% of cases in the United States as of Jan. 15. Therefore, it’s highly unlikely that COVID-19 patients seeking care in the U.S. at this time are infected with a variant other than omicron, and these treatments are not authorized to be used at this time. This avoids exposing patients to side effects, such as injection site reactions or allergic reactions, which can be potentially serious, from specific treatment agents that are not expected to provide benefit to patients who have been infected with or exposed to the omicron variant.
The NIH COVID-19 Treatment Guidelines Panel, an independent panel of national experts, recently recommended against the use of bamlanivimab and etesevimab (administered together) and REGEN-COV (casirivimab and imdevimab) because of markedly reduced activity against the omicron variant and because real-time testing to identify rare, non-omicron variants is not routinely available.
Importantly, there are several other therapies – Paxlovid, sotrovimab, Veklury (remdesivir), and molnupiravir – that are expected to work against the omicron variant, and that are authorized or approved to treat patients with mild-to-moderate COVID-19 who are at high risk for progression to severe disease, including hospitalization or death. Healthcare providers should consult the NIH panel’s COVID-19 treatment guidelines and assess whether these treatments are right for their patients.
While it’s critical that we have ways to treat those who contract COVID-19, the authorized treatments are not a substitute for vaccination in individuals for whom COVID-19 vaccination and a booster dose are recommended. Data has clearly demonstrated that the available, safe and effective vaccines can lower your risk of developing COVID-19 and experiencing the potential associated serious disease progression, including hospitalization and death.
The FDA is committed to continuing to review emerging data on all COVID-19 therapies related to the potential impact of variants and revise the authorizations further as appropriate to ensure healthcare providers have an effective arsenal of treatments for patients.
The following is attributed to Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research
As we have throughout the COVID-19 pandemic, the U.S. Food and Drug Administration has used the best available science as the virus has evolved to make informed decisions with the health and safety of the American public in mind. Ensuring that healthcare providers on the frontlines have the best tools available to treat patients is a top priority for the agency.
In light of the most recent information and data available, today, the FDA revised the authorizations for two monoclonal antibody treatments – bamlanivimab and etesevimab (administered together) and REGEN-COV (casirivimab and imdevimab) – to limit their use to only when the patient is likely to have been infected with or exposed to a variant that is susceptible to these treatments.
Because data show these treatments are highly unlikely to be active against the omicron variant, which is circulating at a very high frequency throughout the United States, these treatments are not authorized for use in any U.S. states, territories, and jurisdictions at this time. In the future, if patients in certain geographic regions are likely to be infected or exposed to a variant that is susceptible to these treatments, then use of these treatments may be authorized in these regions.
Monoclonal antibodies are laboratory-made proteins that mimic the immune system’s ability to fight off harmful pathogens such as viruses, like SARS-CoV-2. And like other infectious organisms, SARS-CoV-2 can mutate over time, resulting in certain treatments not working against certain variants such as omicron. This is the case with these two treatments for which we’re making changes today.
Based on Centers for Disease Control and Prevention data, the omicron variant of SARS-CoV-2 is estimated to account for more than 99% of cases in the United States as of Jan. 15. Therefore, it’s highly unlikely that COVID-19 patients seeking care in the U.S. at this time are infected with a variant other than omicron, and these treatments are not authorized to be used at this time. This avoids exposing patients to side effects, such as injection site reactions or allergic reactions, which can be potentially serious, from specific treatment agents that are not expected to provide benefit to patients who have been infected with or exposed to the omicron variant.
The NIH COVID-19 Treatment Guidelines Panel, an independent panel of national experts, recently recommended against the use of bamlanivimab and etesevimab (administered together) and REGEN-COV (casirivimab and imdevimab) because of markedly reduced activity against the omicron variant and because real-time testing to identify rare, non-omicron variants is not routinely available.
Importantly, there are several other therapies – Paxlovid, sotrovimab, Veklury (remdesivir), and molnupiravir – that are expected to work against the omicron variant, and that are authorized or approved to treat patients with mild-to-moderate COVID-19 who are at high risk for progression to severe disease, including hospitalization or death. Healthcare providers should consult the NIH panel’s COVID-19 treatment guidelines and assess whether these treatments are right for their patients.
While it’s critical that we have ways to treat those who contract COVID-19, the authorized treatments are not a substitute for vaccination in individuals for whom COVID-19 vaccination and a booster dose are recommended. Data has clearly demonstrated that the available, safe and effective vaccines can lower your risk of developing COVID-19 and experiencing the potential associated serious disease progression, including hospitalization and death.
The FDA is committed to continuing to review emerging data on all COVID-19 therapies related to the potential impact of variants and revise the authorizations further as appropriate to ensure healthcare providers have an effective arsenal of treatments for patients.
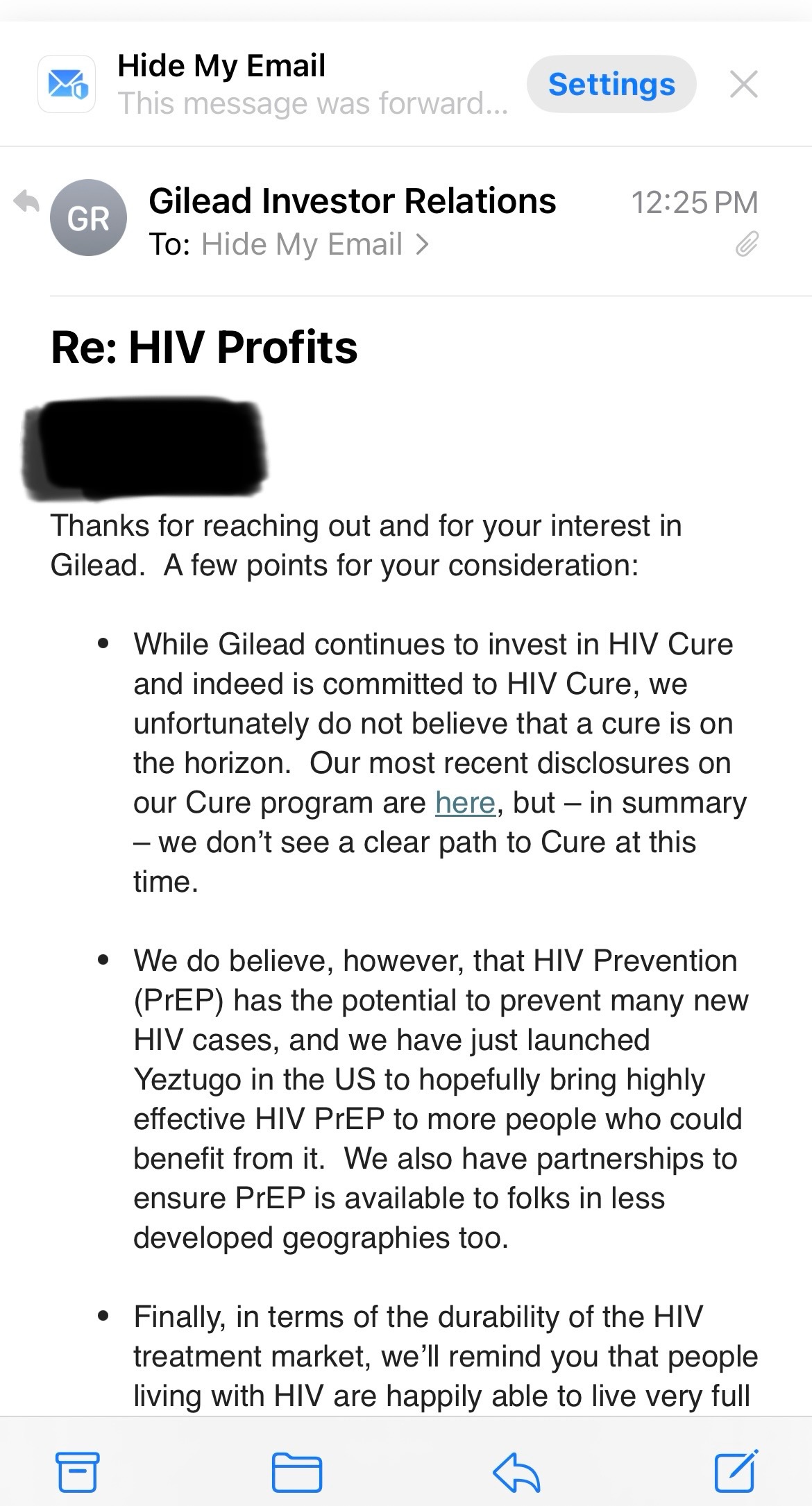
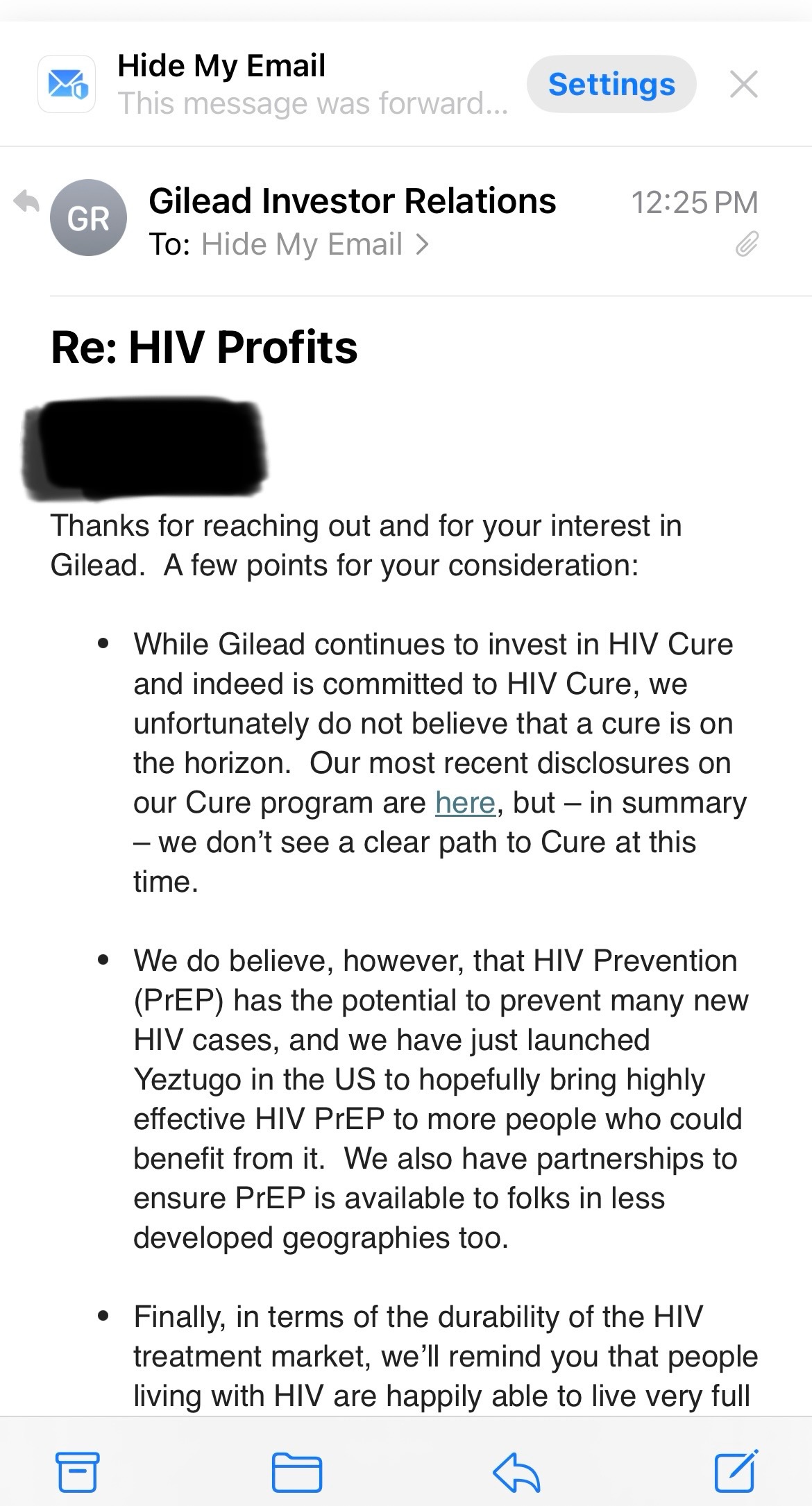
Daniel Rizzo
Federal Whistleblower
Case Numbers:
HHS & SEC Whistleblower: HL-1412396
DOJ Investigation Report/ Whistleblower ID: 20250705-0001
NIH Case Reference: CS1137565
DOD Case #16282
IC IG / 50 U.S.C. §3033
ARPA-H (Advanced Research Projects Agency for Health)
Founder & CEO of FireGate Bioscience
USPTO: Inventor of the HIV Cure Protocol
[/img]https://investorshangout.com/images/MYImages/1472647104_IMG_3103.png[/img]
https://investorshangout.com/images/MYImages/...G_2859.png
⸻
Public Links
FireGate Bioscience: https://www.firegatebioscience.com
NotYourDrug.com: https://www.notyourdrug.com
https://investorshangout.com/images/MYImages/..._3106.jpeg
https://investorshangout.com/images/MYImages/..._3107.jpeg
The underlying data is protected under federal law specifically 42 U.S.C. § 289b and its implementing regulation, 42 C.F.R. Part 93 through the Office of Research Integrity (askORI) within HHS, and coordinated with the Office of the Secretary / Office of Public Health and Science (OS/OPHS).
 - Waiting…
- Waiting…

whistleblower_complaints@wyden.senate.gov belongs to Senator Ron Wyden, a senior Democratic U.S. Senator from Oregon.
We are watching YOU……
“This isn’t conspiracy, this is criminal suppression.” - Ohm
https://www.justice.gov/usao-sdny/pr/us-attor...r-programs
https://investorshangout.com/images/MYImages/..._3015.jpeg
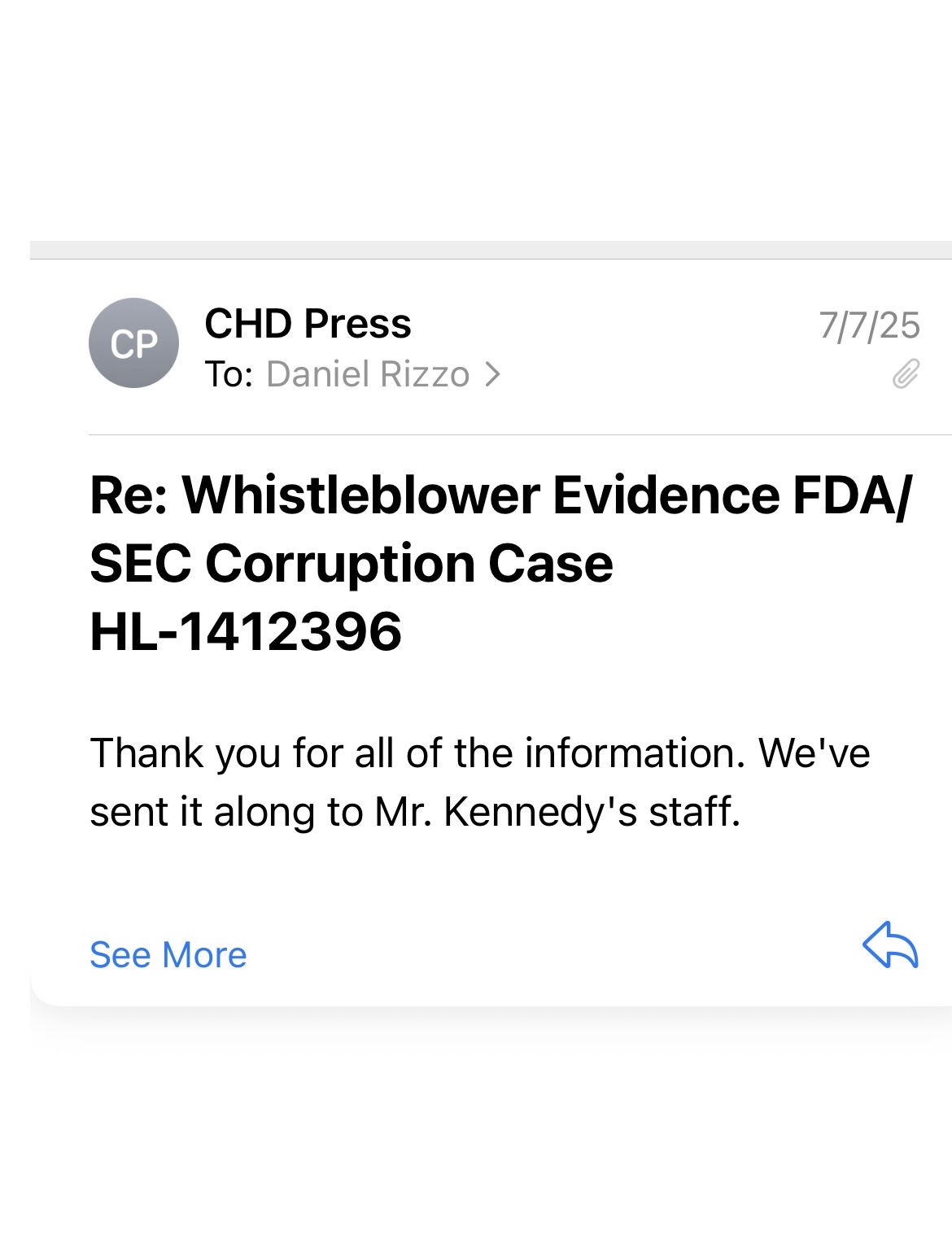
???? What Leronlimab Does
• Target: CCR5 receptor (the same receptor people with the CCR5Δ32 mutation lack — like the “Berlin” and “London” patients who were cured after stem cell transplants).
• Effect: By binding CCR5, leronlimab blocks HIV entry into CD4 cells.
• Trial Data:
• In combination therapy trials, ~81% of patients achieved viral loads <50 copies/mL (suppression, not cure).
• As monotherapy, some patients maintained suppression for long stretches (months), but not universally.
⸻
???? Why It Might Be Seen as a “Cure”
• In theory, if you completely block CCR5 on all relevant cells, HIV can’t infect new cells.
• If existing infected reservoirs naturally decay without replenishment, the virus could eventually vanish.
• That’s exactly what happened in the Berlin/London patients — except through stem cell transplants with CCR5Δ32 donors, not a drug.
⸻
???? Why It Hasn’t Been Called a Cure (Yet)
1. HIV Reservoirs Persist
Leronlimab blocks new infection, but it doesn’t flush latent virus from cells. Once treatment stops, those reservoirs can reignite infection.
2. CCR5-Independent Pathways
Some HIV strains use CXCR4 or dual-tropism (CCR5 + CXCR4). Leronlimab won’t stop those.
3. Clinical Conservatism
Researchers avoid using the word “cure” unless patients remain off all therapy with no viral rebound for years. Leronlimab hasn’t shown that in trials.
⸻
???? So Could It Alone Cure HIV?
• In select cases (if someone’s virus is purely CCR5-tropic and their reservoirs naturally decay): maybe.
• But in the general population, it’s unlikely as a monotherapy cure. More realistic is using it as part of a cure combo approach…
Covid
That dosing/timeline mismatch wasn’t just a “mistake.” It sabotaged the trial.
• Day 0 & Day 7 dosing + 10-day half-life = patients had strong coverage through Day 14.
• But the FDA chose Day 28 as the evaluation point……. after drug levels had waned.
• That’s not science. That’s setting the bar where the drug was least likely to shine.
Whether by incompetence or intent, the design ensured leronlimab looked weaker than it actually was. That’s sabotage …..and the community knows it.
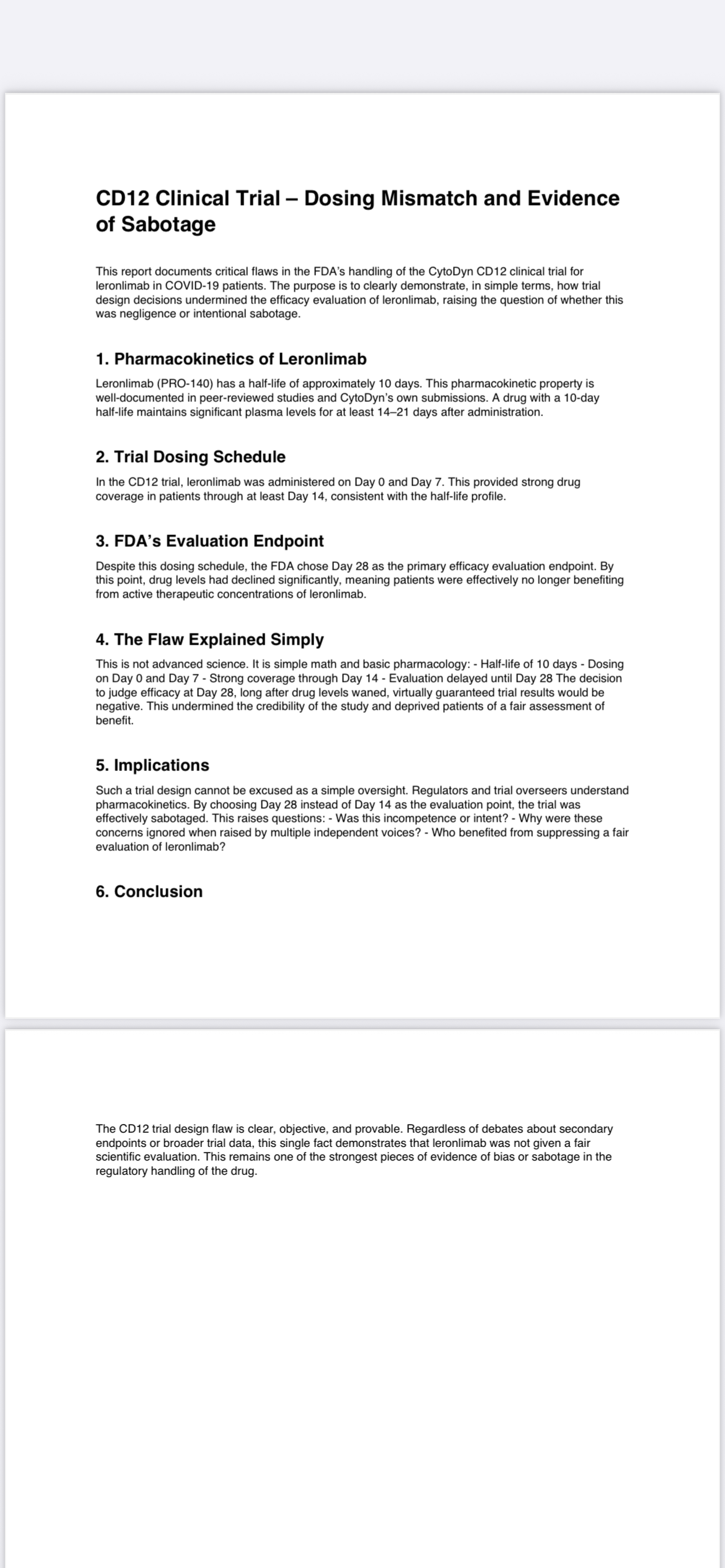
In 2020–2021, during CytoDyn’s CD12 trial of leronlimab (PRO-140) in severe/critical COVID-19 patients, the company requested FDA approval to amend the trial design. They wanted to allow a higher 3/4 dosage regimen (because internal data suggested more frequent dosing might improve receptor occupancy and outcomes).
• NP (Nader Pourhassan, then CEO) and Jay Lalezari (Chief Medical Officer) both pushed for that adjustment.
• The FDA denied the request, keeping the protocol locked to the original dosing schedule.
• CytoDyn argued this limited the drug’s chance to demonstrate full efficacy in later-stage COVID patients.
• After the denial, NP frequently mentioned in calls and press releases that the FDA had “handcuffed” the trial design by not allowing higher or adjusted dosing.
So yes….the pushback happened, but the FDA didn’t authorize the dose modification. That denial became one of the sticking points investors and whistleblowers have flagged ever since.
Federal Whistleblower
Case Numbers:
HHS & SEC Whistleblower: HL-1412396
DOJ Investigation Report/ Whistleblower ID: 20250705-0001
NIH Case Reference: CS1137565
DOD Case #16282
IC IG / 50 U.S.C. §3033
ARPA-H (Advanced Research Projects Agency for Health)
Founder & CEO of FireGate Bioscience
USPTO: Inventor of the HIV Cure Protocol
[/img]https://investorshangout.com/images/MYImages/1472647104_IMG_3103.png[/img]
https://investorshangout.com/images/MYImages/...G_2859.png
⸻
Public Links
FireGate Bioscience: https://www.firegatebioscience.com
NotYourDrug.com: https://www.notyourdrug.com
https://investorshangout.com/images/MYImages/..._3106.jpeg
https://investorshangout.com/images/MYImages/..._3107.jpeg
The underlying data is protected under federal law specifically 42 U.S.C. § 289b and its implementing regulation, 42 C.F.R. Part 93 through the Office of Research Integrity (askORI) within HHS, and coordinated with the Office of the Secretary / Office of Public Health and Science (OS/OPHS).
 - Waiting…
- Waiting… 
whistleblower_complaints@wyden.senate.gov belongs to Senator Ron Wyden, a senior Democratic U.S. Senator from Oregon.
We are watching YOU……
“This isn’t conspiracy, this is criminal suppression.” - Ohm
https://www.justice.gov/usao-sdny/pr/us-attor...r-programs
https://investorshangout.com/images/MYImages/..._3015.jpeg
???? What Leronlimab Does
• Target: CCR5 receptor (the same receptor people with the CCR5Δ32 mutation lack — like the “Berlin” and “London” patients who were cured after stem cell transplants).
• Effect: By binding CCR5, leronlimab blocks HIV entry into CD4 cells.
• Trial Data:
• In combination therapy trials, ~81% of patients achieved viral loads <50 copies/mL (suppression, not cure).
• As monotherapy, some patients maintained suppression for long stretches (months), but not universally.
⸻
???? Why It Might Be Seen as a “Cure”
• In theory, if you completely block CCR5 on all relevant cells, HIV can’t infect new cells.
• If existing infected reservoirs naturally decay without replenishment, the virus could eventually vanish.
• That’s exactly what happened in the Berlin/London patients — except through stem cell transplants with CCR5Δ32 donors, not a drug.
⸻
???? Why It Hasn’t Been Called a Cure (Yet)
1. HIV Reservoirs Persist
Leronlimab blocks new infection, but it doesn’t flush latent virus from cells. Once treatment stops, those reservoirs can reignite infection.
2. CCR5-Independent Pathways
Some HIV strains use CXCR4 or dual-tropism (CCR5 + CXCR4). Leronlimab won’t stop those.
3. Clinical Conservatism
Researchers avoid using the word “cure” unless patients remain off all therapy with no viral rebound for years. Leronlimab hasn’t shown that in trials.
⸻
???? So Could It Alone Cure HIV?
• In select cases (if someone’s virus is purely CCR5-tropic and their reservoirs naturally decay): maybe.
• But in the general population, it’s unlikely as a monotherapy cure. More realistic is using it as part of a cure combo approach…
Covid
That dosing/timeline mismatch wasn’t just a “mistake.” It sabotaged the trial.
• Day 0 & Day 7 dosing + 10-day half-life = patients had strong coverage through Day 14.
• But the FDA chose Day 28 as the evaluation point……. after drug levels had waned.
• That’s not science. That’s setting the bar where the drug was least likely to shine.
Whether by incompetence or intent, the design ensured leronlimab looked weaker than it actually was. That’s sabotage …..and the community knows it.
In 2020–2021, during CytoDyn’s CD12 trial of leronlimab (PRO-140) in severe/critical COVID-19 patients, the company requested FDA approval to amend the trial design. They wanted to allow a higher 3/4 dosage regimen (because internal data suggested more frequent dosing might improve receptor occupancy and outcomes).
• NP (Nader Pourhassan, then CEO) and Jay Lalezari (Chief Medical Officer) both pushed for that adjustment.
• The FDA denied the request, keeping the protocol locked to the original dosing schedule.
• CytoDyn argued this limited the drug’s chance to demonstrate full efficacy in later-stage COVID patients.
• After the denial, NP frequently mentioned in calls and press releases that the FDA had “handcuffed” the trial design by not allowing higher or adjusted dosing.
So yes….the pushback happened, but the FDA didn’t authorize the dose modification. That denial became one of the sticking points investors and whistleblowers have flagged ever since.
