(Total Views: 1491)
Posted On: 03/02/2021 1:25:46 PM
Post# of 158017

Long Hauler (LH) will be a VERY important condition and market in the future.
Our success or not will depend on whether our only drug does indeed plays a (positive) role in this.
Dr. Patterson has been doing lots of research in this area.
From his paper (a good read) very interesting conclusions can be drawn:
https://www.biorxiv.org/content/10.1101/2020....122v1.full
He performed quantitative, multiplex cytokine/chemokine panels on 30 normal individuals and then compared with 64 long haulers measuring cytokine/chemokine profiles. He found IL-2, IL-4, CCL3, IL-6, IL-10, IFN-γ, and VEGF were all significantly elevated compared to normal controls and that GM-CSF and CCL4 were significantly lower than normal controls.
Also, he found a significant decrease in T regulatory cells compared to normal individuals.
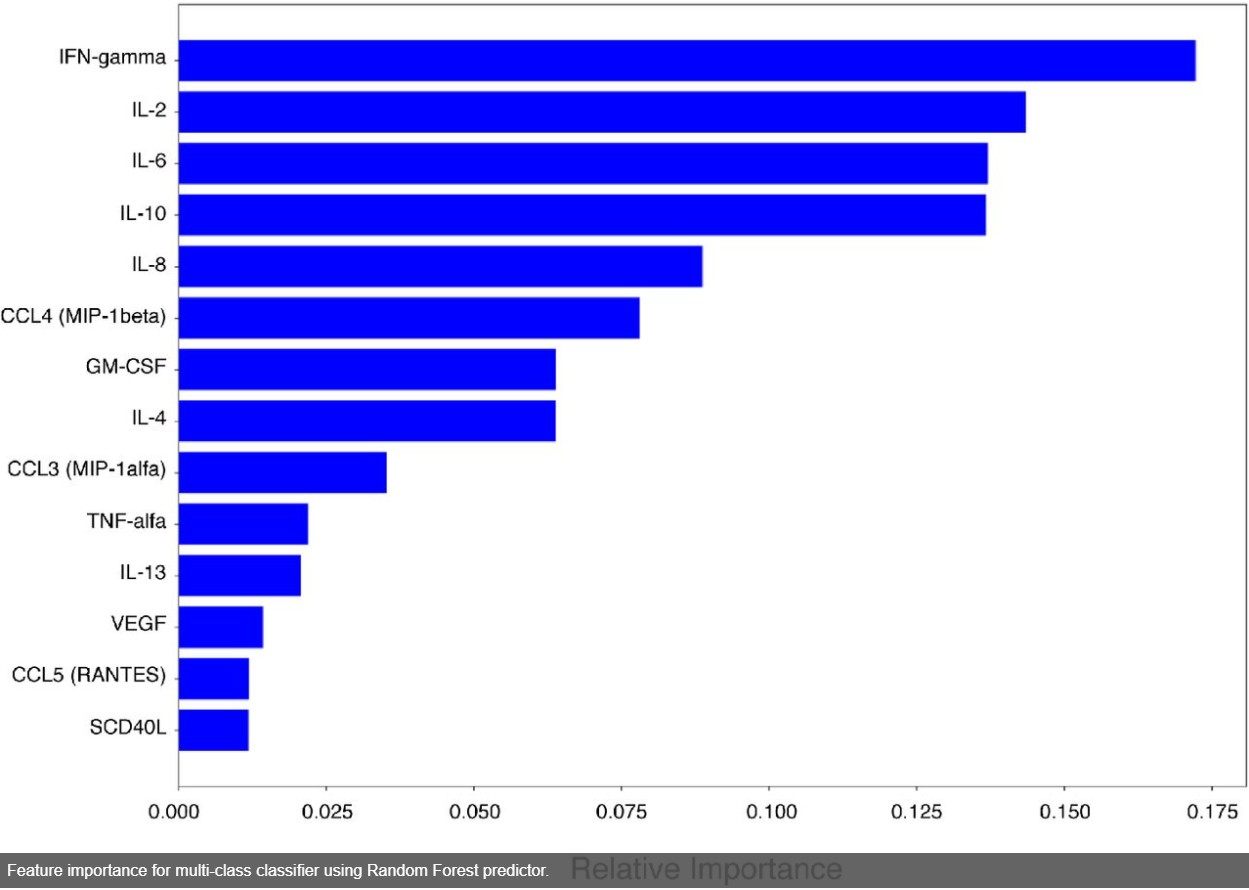
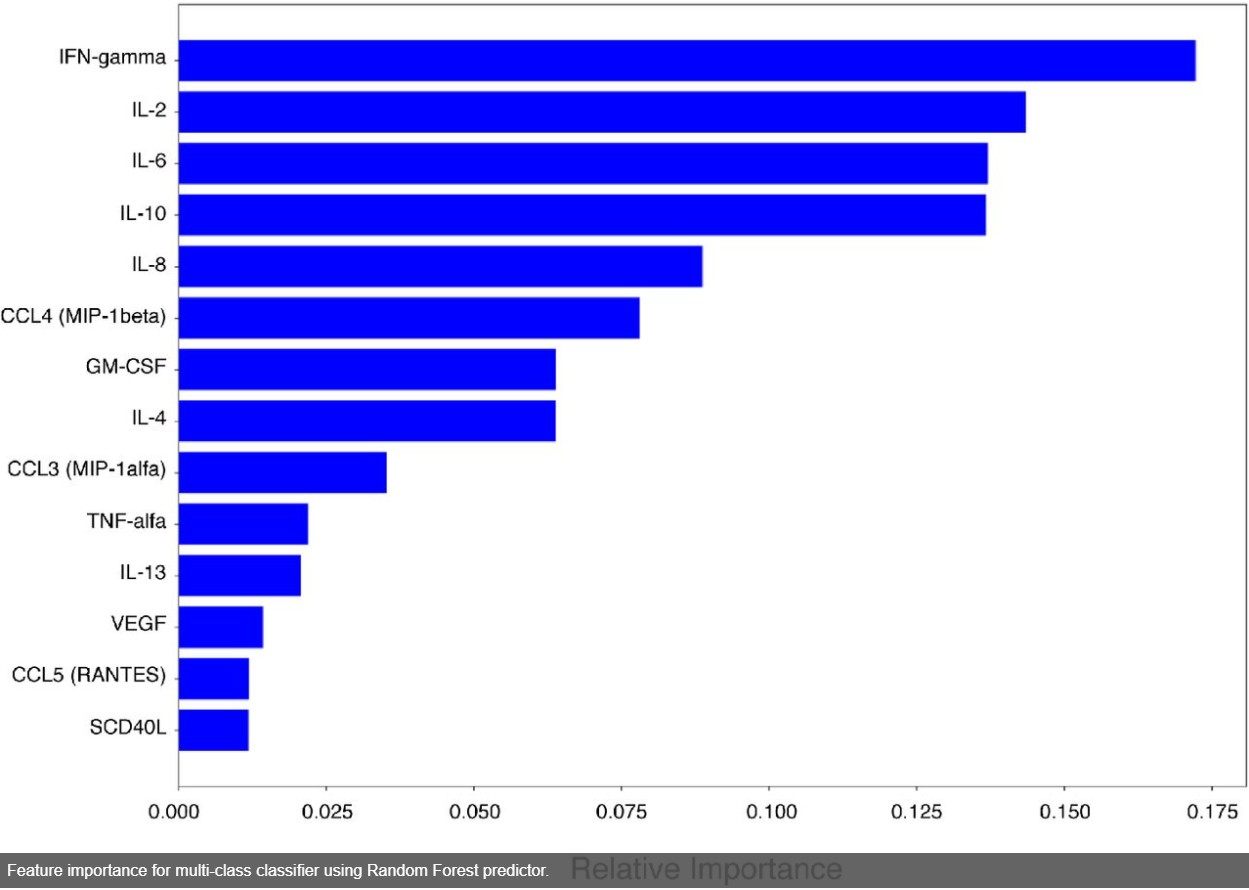
The picture shows his model in an attempt to identify the most relevant or informative features.
They then defined a chronic COVID-19 formula:
S1 = (IFN-γ + IL-2)/ CCL4-MIP-1β
How does this affects us ?? It is not a big discovery that IFN-γ and IL-2 are elevated, and depict the condition as they are the hallmarks of the body response in trying to activate pro-inflammatory effector T cells with the objective of generating an effective immune response to eliminate the COVID virus.
However, as Dr. Patterson elaborates, the problem is that, once this happens the induced inflammation is not efficient clearing the virus if there are not enough recruitment signals to attract activated T cells. Therefore the symptoms persists.
The key lies in that the count of CCL4 is low (hence the formula has it in the denominator). Low CCL4 interfere with the polarization and hinders the activated T cell recruitment.
So, when the levels of RANTES are high and there is low count of CCL4 (CCR1-antagonist) there is a higher recruitment of myeloid cells expressing CCR1 which, in the context of COVID is resulting in high levels of IFN-γ (and IL-2).
Dr. Patterson concludes in his study:
So, Dr Patterson is advocating to target CCL-4 and, is an obvious conclusion, after his neural model output this value in the denominator and his measurements indicated low concentrations in LH. The bottom line, if CCL-4 can be increased and, hopefully, if as well IFN-γ and IL-2 are reduced (as an indication of virus reduction), the person is not a LH anymore.
The beauty of this all is that CCL-4 can signal only trough CCR-5 (as opposed to RANTES which can signal through CCR1 and CCR3 as well). Therefore a CCR-5 antagonist will disrupt CCL-4 which in turn will affect CCR1 (upregulated in COVID) whose expression is associated with IFN-γ and IL-2.
So, our little molecule will have a prime position in the LH COVID battle in the future if Dr. Patterson’s results are correct, and I don’t doubt they are.
Our success or not will depend on whether our only drug does indeed plays a (positive) role in this.
Dr. Patterson has been doing lots of research in this area.
From his paper (a good read) very interesting conclusions can be drawn:
https://www.biorxiv.org/content/10.1101/2020....122v1.full
He performed quantitative, multiplex cytokine/chemokine panels on 30 normal individuals and then compared with 64 long haulers measuring cytokine/chemokine profiles. He found IL-2, IL-4, CCL3, IL-6, IL-10, IFN-γ, and VEGF were all significantly elevated compared to normal controls and that GM-CSF and CCL4 were significantly lower than normal controls.
Also, he found a significant decrease in T regulatory cells compared to normal individuals.
The picture shows his model in an attempt to identify the most relevant or informative features.
They then defined a chronic COVID-19 formula:
S1 = (IFN-γ + IL-2)/ CCL4-MIP-1β
How does this affects us ?? It is not a big discovery that IFN-γ and IL-2 are elevated, and depict the condition as they are the hallmarks of the body response in trying to activate pro-inflammatory effector T cells with the objective of generating an effective immune response to eliminate the COVID virus.
However, as Dr. Patterson elaborates, the problem is that, once this happens the induced inflammation is not efficient clearing the virus if there are not enough recruitment signals to attract activated T cells. Therefore the symptoms persists.
The key lies in that the count of CCL4 is low (hence the formula has it in the denominator). Low CCL4 interfere with the polarization and hinders the activated T cell recruitment.
So, when the levels of RANTES are high and there is low count of CCL4 (CCR1-antagonist) there is a higher recruitment of myeloid cells expressing CCR1 which, in the context of COVID is resulting in high levels of IFN-γ (and IL-2).
Dr. Patterson concludes in his study:
Quote:
Interestingly, COVID-19 individuals (including LH, mild, severe) show high levels of CCL5, a chemoattractant that like CCL4 signals through CCR5. Indeed, the disruption of the CCL5-CCR5 pathway restores immune balance in critical COVID-19 patients. In the specific case of LH, despite the high concentrations of CCL5 a reduction on the CCL4-mediated recruitment of activated T cells is proposed.
So, Dr Patterson is advocating to target CCL-4 and, is an obvious conclusion, after his neural model output this value in the denominator and his measurements indicated low concentrations in LH. The bottom line, if CCL-4 can be increased and, hopefully, if as well IFN-γ and IL-2 are reduced (as an indication of virus reduction), the person is not a LH anymore.
The beauty of this all is that CCL-4 can signal only trough CCR-5 (as opposed to RANTES which can signal through CCR1 and CCR3 as well). Therefore a CCR-5 antagonist will disrupt CCL-4 which in turn will affect CCR1 (upregulated in COVID) whose expression is associated with IFN-γ and IL-2.
So, our little molecule will have a prime position in the LH COVID battle in the future if Dr. Patterson’s results are correct, and I don’t doubt they are.
