(Total Views: 611)
Posted On: 05/31/2019 3:05:16 PM
Post# of 158169
Quiet day, so I spent a little time looking into mouse models in hopes to find out how likely preclinical results translate into clinical success. I looked into this some previously when the 98% TNBC results were first announced and recall results varied greatly and have read other articles or statements that state 90% success. Still non-conclusive to me, but hopefully our wait isn't much longer.
Here is a brief comparison of 3 of the most widely used for cancer studies:
Insert-tag-herehttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC2562196/
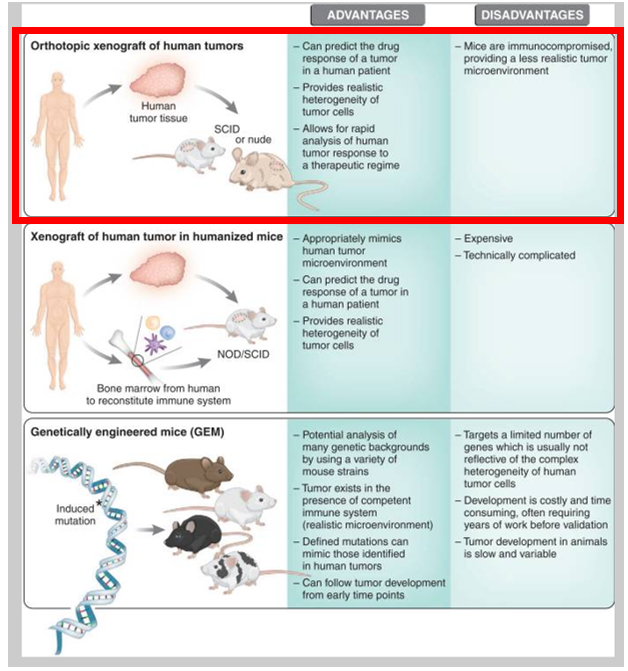
Per our PRs and listening to RP interviews, we are using a xenograft mouse models in which breast cancer was put into mice (I believe the xenograft model highlighted above). Here is a good article that compares these models. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2562196/
" The effect of a drug on the rate of tumor growth or cytostasis has been reported to often be more predictive of a clinical response than tumor shrinkage/regression (Kelland, 2004). Moreover, subcutaneous tumor models that are not orthotopic and do not represent appropriate sites for human tumors are not predictive when used to test responses to anti-cancer drugs (Killion et al., 1998). A challenge presented with orthotopic models, as compared with subcutaneous models, is the difficulty of following tumor growth. However, the recent development of new magnetic resonance imaging (MRI) and micro-imaging techniques may minimize this problem."
However, if we are using humanized mice (middle model) this is likely even better as "these immunological deficits can, in principle, be largely overcome by grafting human tumors onto ‘humanized’ NOD/SCID mice."
In summary, both the orthotopic human tumor xenograft and the GEM models are useful for enhancing our understanding of cancer development and treatment. Each has its strengths and limitations, with the orthotopic human tumor xenograft being excellent for predicting drug response in human tumors, and the GEM model being best for examining the role of specific genes in tumor development and progression. Whichever model is used to predict clinical response in patients, it is important to get at least a 50% inhibition in tumor growth to achieve a qualified ‘response’ to therapy, and to use clinically relevant dosages of therapeutic agents and monitor survival. In addition, it is important to determine whether tumor growth returns when the drug is discontinued, and, if so, whether the re-growth is faster when treatment is paused compared with before the treatment began. If this is the case, in spite of any response to drug therapy, the rebound effect advises against use of that drug treatment regime for tumor types exhibiting a rebound effect. In conclusion, we do not have ideal murine models of human tumors, but must learn to interpret our data within the framework of the limitations of the assay used.
Here is a brief comparison of 3 of the most widely used for cancer studies:
Insert-tag-herehttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC2562196/
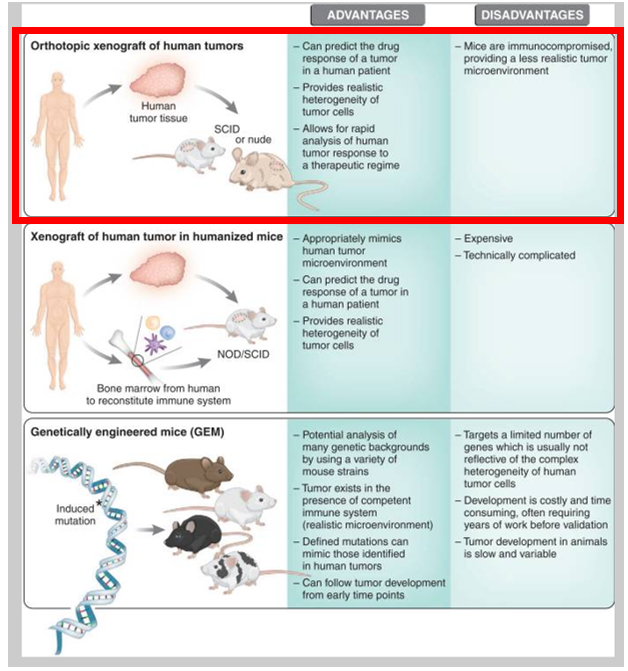
Per our PRs and listening to RP interviews, we are using a xenograft mouse models in which breast cancer was put into mice (I believe the xenograft model highlighted above). Here is a good article that compares these models. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2562196/
" The effect of a drug on the rate of tumor growth or cytostasis has been reported to often be more predictive of a clinical response than tumor shrinkage/regression (Kelland, 2004). Moreover, subcutaneous tumor models that are not orthotopic and do not represent appropriate sites for human tumors are not predictive when used to test responses to anti-cancer drugs (Killion et al., 1998). A challenge presented with orthotopic models, as compared with subcutaneous models, is the difficulty of following tumor growth. However, the recent development of new magnetic resonance imaging (MRI) and micro-imaging techniques may minimize this problem."
However, if we are using humanized mice (middle model) this is likely even better as "these immunological deficits can, in principle, be largely overcome by grafting human tumors onto ‘humanized’ NOD/SCID mice."
In summary, both the orthotopic human tumor xenograft and the GEM models are useful for enhancing our understanding of cancer development and treatment. Each has its strengths and limitations, with the orthotopic human tumor xenograft being excellent for predicting drug response in human tumors, and the GEM model being best for examining the role of specific genes in tumor development and progression. Whichever model is used to predict clinical response in patients, it is important to get at least a 50% inhibition in tumor growth to achieve a qualified ‘response’ to therapy, and to use clinically relevant dosages of therapeutic agents and monitor survival. In addition, it is important to determine whether tumor growth returns when the drug is discontinued, and, if so, whether the re-growth is faster when treatment is paused compared with before the treatment began. If this is the case, in spite of any response to drug therapy, the rebound effect advises against use of that drug treatment regime for tumor types exhibiting a rebound effect. In conclusion, we do not have ideal murine models of human tumors, but must learn to interpret our data within the framework of the limitations of the assay used.
Please do your own due diligence. All my posts and comments are not to be considered investment advice.
